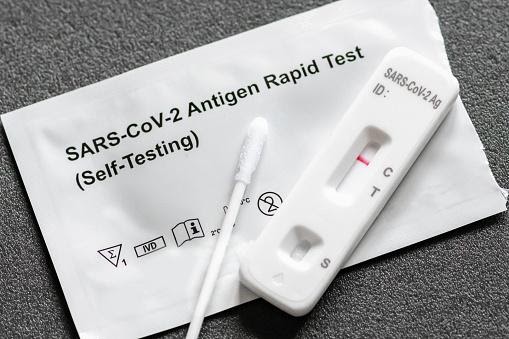
Rapid antigen tests for coronavirus
Rapid antigen tests are intended to determine an individual’s infectious status in a matter of minutes. Are they going to be game-changers?
The United States leads the world in COVID-19 deaths but lags behind a number of countries, large and small, in terms of testing capacity. That could change in the near future.
The US Food and Drug Administration (FDA) granted emergency use approval to a new credit-card-sized coronavirus testing device that costs $5, provides results in 15 minutes, and does not require a laboratory or processing machine. The United States is spending $760 million on 150 million of these amazing rapid antigen tests from Abbott Laboratories, based in Abbott Park, Illinois. Abbott Laboratories plans to increase production to 50 million per month in October.
The rapid antigen tests look for specific proteins on the surface of the virus called antigens and can identify individuals who are at the peak of infection when virus levels in the body are most likely to be high. According to proponents, this could be a game changer. Antigen tests may help avert a pandemic, as they can be administered in large numbers and can identify those most at risk of spreading the disease. These rapid antigen tests are also a critical component of other countries’ testing strategies, such as India and Italy.
Antigen assays are significantly faster and less expensive than gold-standard rapid antigen tests that employ a technique called the polymerase chain reaction to detect viral RNA (PCR). However, antigen tests are not as sensitive as polymerase chain reaction (PCR) rapid antigen tests, which can detect trace amounts of the SARS-CoV-2 virus that causes COVID-19. Click here to check some of the common questions that people usually ask about the rapid test.
This discrepancy concerns some specialists, who fear that antigen tests will miss infectious individuals, resulting in outbreaks in countries where coronavirus transmission is largely controlled. Others view the lower sensitivity as an advantage, as some individuals who receive positive PCR test results are infected but no longer capable of spreading the virus. As a result, antigen tests may shift the emphasis to identifying the most infectious individuals.
While antigen tests are now given by skilled specialists, several businesses are developing versions that are easy enough to conduct at home — similar to pregnancy tests.
“Speeding up, lowering the cost, and simplifying the rapid antigen tests is unquestionably the aim — and I believe the antigen test is the method to do that,” says Martin Burke, a chemist at the University of Illinois at Urbana-Champaign who is co-developing quick diagnostics, including antigen-based assays. “This is by no means the ideal option; it is just the quickest way to get started at the moment,” he explains.
What kind of rapid antigen tests are available and how do they work?
COVID-19 testing is classified into two types: diagnostic rapid antigen tests such as polymerase chain reaction (PCR) and antigen assays that identify components of the SARS-CoV-2 virus, and antibody rapid antigen tests that detect molecules produced by infected individuals. Antibodies form many days after infection and often remain in the blood for weeks after recovery, making antibody testing ineffective for diagnosis (see ‘Catching COVID-19’).
When given appropriately, high-sensitivity polymerase chain reaction (PCR) rapid antigen tests are almost 100 percent accurate in detecting infected individuals. However, such rapid antigen tests often need experienced workers, specialized reagents, and costly machinery that take hours to complete.
While countries such as South Korea and New Zealand have increased PCR-based testing, scaling these rapid antigen tests up has proven problematic in other countries. For example, the United States has experienced a sluggish and poorly organized response to outbreaks, as well as inaccurate testing from the Centers for Disease Control and Prevention (CDC) and supply chain issues. All of this has hampered attempts to collect and prepare samples for PCR, resulting in days or even weeks of waiting periods. These delays, along with a dearth of testing, have aided in the rapid spread of COVID-19 throughout the nation, which had claimed about 200,000 lives by 16 September.
A normal antigen test begins with a health care provider swabbing the back of the patient’s nose or throat — but firms are creating kits that gather saliva samples, which are simpler and safer to obtain than a swab. The sample is then incubated in a solution that ruptures the virus and liberates certain viral proteins. The mixture is then put to a paper strip coated with an antibody specific for these proteins, which are present in the solution. Positive test results are shown by a bright light or a dark band on the paper strip.
Rapid antigen tests provide findings in less than 30 minutes, do not need laboratory processing, and are inexpensive to make. However, such speed comes at a cost in terms of sensitivity. While a standard PCR test may identify a single molecule of RNA in a microlitre of the solution, antigen assays need hundreds — if not tens of thousands — of virus particles per microlitre to get a positive result. As a consequence, if a person has very low virus levels in their body, the test may provide a false-negative result.
When used on individuals who tested positive for SARS-CoV-2 by a routine PCR test, Abbott’s antigen assay detected the virus in 95–100% of cases when samples were taken within a week of the beginning of symptoms. However, this percentage decreased to 75% when samples were obtained more than a week after individuals initially manifested symptoms. The sensitivity — or percentage of accurately identifying infections — of the other antigen tests used in the United States ranges between 84 and 98 percent when a person is tested within a week of exhibiting symptoms.
Other rapid antigen tests that are quicker, cheaper, and more user-friendly than typical PCR assays are also being developed by companies and university research institutes, however they are not being commercialized on the same scale as antigen testing. Several of these additional assays use the gene-editing technique CRISPR to isolate coronavirus genomic bits. Others are faster variations of the PCR test that do not need the same chemicals, which means they are not constrained by the same supply-chain issues. For example, saliva-based polymerase chain reaction (PCR) assays are employed as screening techniques at colleges and by professional basketball teams.